Blue Options gives you great benefits, including coverage for preventive care, prescriptions, and medical emergencies.
But, unlike other plans, Blue Options lets you control your costs every time you get care. You can choose from more than 17,000 doctors and hospital in three benefits tiers. Your cost is based on the tier of primary care provider (PCP) or hospital you choose. And if you need help using your Blue Options plan, we're right there to guide you.
Learn Blue Options in minutes
Understand Doctor and Hospital Tiers
PCPs and hospitals in the Blue Options network are grouped into three benefit levels—or tiers. The tiers are based on cost and nationally accepted standards for quality. The cost you pay for care Out-of-Pocket is based on the benefits tiers of your doctors and hospitals.
| Benefits Tier | Quality | Your Cost |
|---|---|---|
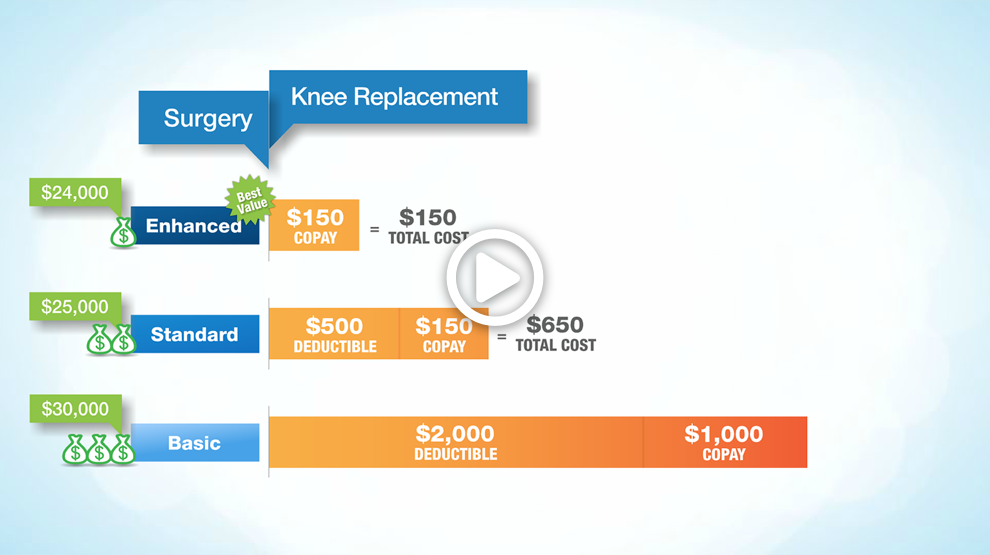
| Enhanced | Includes Massachusetts hospitals and PCPs that meet the standards for quality and low cost relative to our benchmark. | $ — lowest cost |
| Standard1 | Includes Massachusetts hospitals and PCPs that meet the standards for quality and are moderate cost relative to our benchmark and hospitals that do not meet the standards for quality but are low or moderate cost relative to our benchmark. | $$ — moderate cost |
| Basic | Includes Massachusetts hospitals that are high cost relative to our benchmark and PCPs that do not meet the standards for quality and/or are high cost relative to our benchmark. | $$$ — highest cost |
Enhanced
|
Quality Includes Massachusetts hospitals and PCPs that meet the standards for quality and low cost relative to our benchmark. |
|
Your Cost $ — lowest cost |
Standard1
|
Quality Includes Massachusetts hospitals and PCPs that meet the standards for quality and are moderate cost relative to our benchmark and hospitals that do not meet the standards for quality but are low or moderate cost relative to our benchmark. |
|
Your Cost $$ — moderate cost |
Basic
|
Quality Includes Massachusetts hospitals that are high cost relative to our benchmark and PCPs that do not meet the standards for quality and/or are high cost relative to our benchmark. |
|
Your Cost $$$ — highest cost |
1. In limited circumstances, to increase your local access, the Standard Benefits Tier includes certain providers whose scores would put them in the Basic Benefits Tier.
Note: PCPs were measured based on their HMO patients as part of their provider group, and hospitals were measured based on their individual facility performance. Provider groups can be composed of an individual provider, or a number of providers who practice together. Tier placement is based on cost and quality benchmarks where measurable data is available. Providers without sufficient data for either cost or quality are placed in the Standard Benefits Tier. PCPs that do not meet benchmarks for one or both of the domains and hospitals that do not meet benchmarks for cost or that use nonstandard reimbursement are placed in the Basic Benefits Tier.
This web site gives general information about our tiered network plan designs. In our tiered plans, members pay different levels of cost share (copayments, coinsurance, and/or deductibles) depending on the benefits tier of the provider furnishing the services. A provider's benefits tier may change. Overall changes to the benefits tiers of providers will happen no more than once each calendar year. For help in finding the benefits tier of a provider, visit Find a Doctor & Estimate Costs and search for the appropriate network.